Jugulotympanic paragangliomas. Surgical technique and experience of the Egas Moniz Hospital
DOI:
https://doi.org/10.34631/sporl.34Keywords:
Glomus Jugulare Tumor, Jugulotympanic paraganglioma, Postoperative complications, Retrospective Studies, Skull base, Temporal Bone, Therapeutic embolization, Treatment outcomeAbstract
Objectives: Describe the surgical technique and experience of the departments of Otolaryngology and Neurosurgery of the Egas Moniz Hospital in the surgical treatment of jugulotympanic paragangliomas.
Study design: Description of the surgical technique and retrospective evaluation of the cases operated in a period of 20 years.
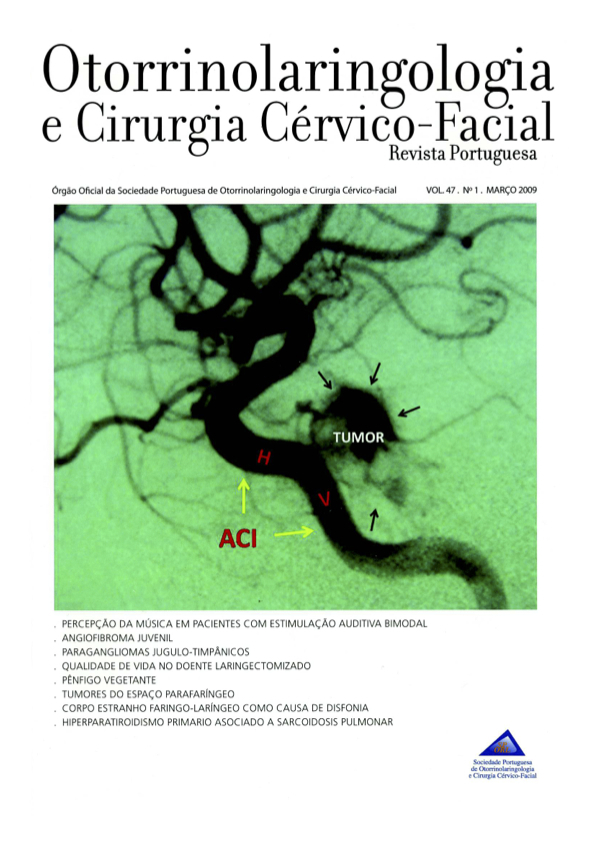
Materials and methods: 24 patients were operated by an otoneurosurgical team between 1988 and 2007 and included in the study. The surgical technique was the Infratemporal Fossa Aproach type A in all the cases. Data were obtained from a recent evaluation of the patients and review of the clinical records. The outcome measures were: clinical manifestations, preoperative embolization and surgical technique, tumor removal, mortality morbidity and evolution of residual lesions.
Results: Clinical presentation was similar to other series. Total removal of the tumor was obtained in 11 (45%) cases. In the majority of the other cases residual disease remained controlled. Two patients died from pneumonia and morbidity was similar to other series.
Conclusions: Infratemporal Fossa Aproach type A is the best surgical technique to remove jugulotympanic para gangliomas, but the treatment of this pathology should be concentrated in referral centers, where differentiated and stable otoneurosurgical teams can control the disease with the less morbidity and mortality