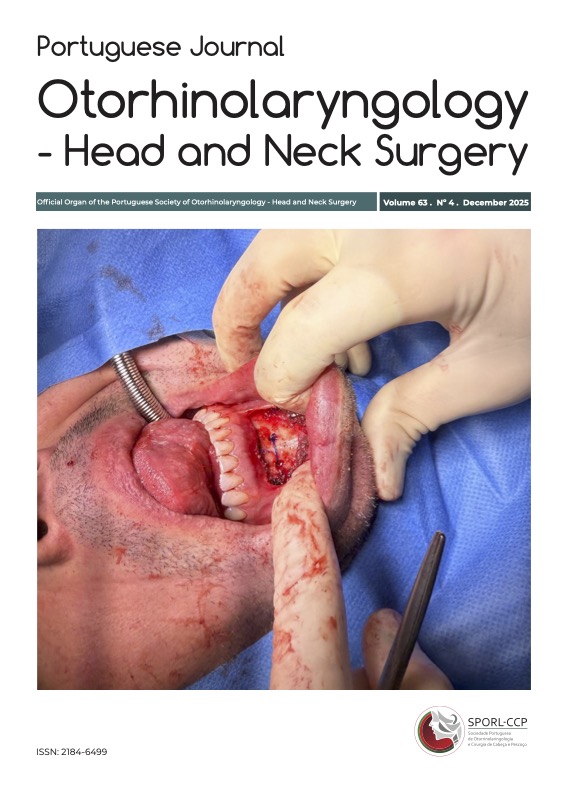
Trans-oral tongue suspension: a promising technique
DOI:
https://doi.org/10.34631/sporl.3098Keywords:
Obstructive sleep apnea, snoring, tongue base suspension, transoral tongue suspensionAbstract
Objectives: Presentation of the outcomes of tongue suspension using the technique described by Hsin et al. (2022), based on a case series of three patients.
Methods: One patient with snoring and two with moderate and severe Obstructive Sleep Apnea (OSA) according to Level III Polysomnography are presented. After identification on DISE of an anteroposterior collapse of the tongue base, Moore B 80–100%, associated with secondary collapse of the epiglottis, the patients underwent tongue suspension surgery following the technique described by Hsin et al.
Results: A good clinical outcome and healing were observed after the procedure, with resolution of both snoring and OSA in all patients. No major complications were reported.
Conclusion: This new technique proved to be safe and effective in treating OSA in adults with retrolingual obstruction. It has low morbidity, is easily performed, and can be integrated into multilevel approaches, expanding the therapeutic options for this condition.
Downloads
References
- Garvey JF, Pengo MF, Drakatos P, Kent BD. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis. 2015 May;7(5):920–929. doi:10.3978/j.issn.2072-1439.2015.04.52.
- Bonsignore MR, Saaresranta T, Riha RL. Sex differences in obstructive sleep apnoea. Eur Respir Rev. 2019;28(154):190030. doi: 10.1183/16000617.0030-2019.
- Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015 Apr;3(4):310–318. doi: 10.1016/S2213-2600(15)00043-0.
- Toh ST, Hsu PP. Robotic obstructive sleep apnea surgery. Adv Otorhinolaryngol. 2017;80:125–135. doi: 10.1159/000470882.
- Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A. Defining phenotypic causes of obstructive sleep apnea: identification of novel therapeutic targets. Am J Respir Crit Care Med. 2013;188(8):996–1004. doi: 10.1164/rccm.201303-0448OC.
- Lin HC, Weaver EM, Lin HS, Friedman M. Multilevel obstructive sleep apnea surgery. Adv Otorhinolaryngol. 2017;80:109–115. doi: 10.1159/000470879.
- Turhan M, Bostanci A. Robotic tongue-base resection combined with tongue-base suspension for obstructive sleep apnea. Laryngoscope. 2020 Sep;130(9):2285–2291. doi: 10.1002/lary.28443.
- Bostanci A, Turhan M. A systematic review of tongue base suspension techniques as an isolated procedure or combined with uvulopalatopharyngoplasty in obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2016 Oct;273(10):2895–2901. doi: 10.1007/s00405-015-3814-3.
- Miller SC, Nguyen SA, Ong AA, Gillespie MB. Transoral robotic base of tongue reduction for obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2017 Jan;127(1):258–265. doi: 10.1002/lary.26060.
- Bacak B, Porterfield L, Karelsky S. Multilevel airway obstruction phenotypes in adult OSA. OTO Open. 2023 Apr-Jun;7(2):e21. doi: 10.1002/oto2.21.
- Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45:43. doi: 10.1186/s40463-016-0156-0.
- Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011 Dec;15(6):343–356. doi: 10.1016/j.smrv.2011.01.003.
- De Vito A, Agnoletti V, Berrettini S, Piraccini E, Criscuolo A, Corso R, Campanini A, Gambale G, Vicini C. The importance of drug-induced sedation endoscopy (D.I.S.E.) techniques in surgical decision making: conventional versus target-controlled infusion techniques—a prospective randomized controlled study and a retrospective surgical outcomes analysis. Eur Arch Otorhinolaryngol. 2017 May;274(5):2307–2317. doi: 10.1007/s00405-016-4447-x.
- Vroegop AV, Vanderveken OM, Boudewyns AN, Scholman J, Saldien V, Wouters K, et al. Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope. 2014 Mar;124(3):797–802. doi: 10.1002/lary.24479.
- Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN. Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg. 2010 Apr;136(4):393–397. doi:10.1001/archoto.2010.26.
- Friedman M, Ibrahim H, Joseph NJ. Prediction of uvulopalatopharyngoplasty outcome: anatomy-based staging system versus severity-based staging system. Laryngoscope. 2004 Oct;114(10):1979–1984. doi:10.1097/01.mlg.0000143153.63075.43
- Calvo-Henriquez C, Boronat-Catala B, Rivero-Fernández I, Cammaroto G, Ibrahim B, Lechien JR. et al. Safety of tongue base procedures for sleep apnoea in adults: a systematic review and meta-analysis from the YO-IFOS study group. Acta Otorrinolaringol Esp (Engl Ed). 2022 Nov-Dec;73(6):384-393. doi: 10.1016/j.otoeng.2021.10.004.Eur
- Lin HC, Hwang MS, Liao CC, Friedman M. Taste disturbance following tongue base resection for OSA. Laryngoscope. 2016 Apr;126(4):1009–1013. doi: 10.1002/lary.25580.
- Hsin L-J, Lee Y-C, Lin W-N, Lu Y-A, Lee L-A, Tsai M-S, et al. Transoral tongue suspension for obstructive sleep apnea—A preliminary study. J Clin Med. 2022 Aug 24;11(17):4960. doi: 10.3390/jcm11174960.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Pedro Barros, João Viana Pinto, Maria Marques Silva, Jorge Rodrigues, Ricardo Vaz, Carla Pinto Moura, Manuel Mendes Leal

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.