Endoscopic resection of invasive glomangiopericytoma following preoperative embolisation: A case report and literature review
DOI:
https://doi.org/10.34631/sporl.568Keywords:
Glomangiopericitoma, embolização, cirurgiaAbstract
Objectives: The sinonasal hemangiopericytomas (SNHPC) are rare tumors, originating from perivascular modified myoepithelial cells, and are often referred as glomangioperycitomas (GPC). These lesions have a rather benign local behavior, with rare metastasis rate but high recurrence rate. Histologically are classified as low-grade malignant lesions. The treatment is the complete excision of the lesion with intraoperative disease free surgical margins.
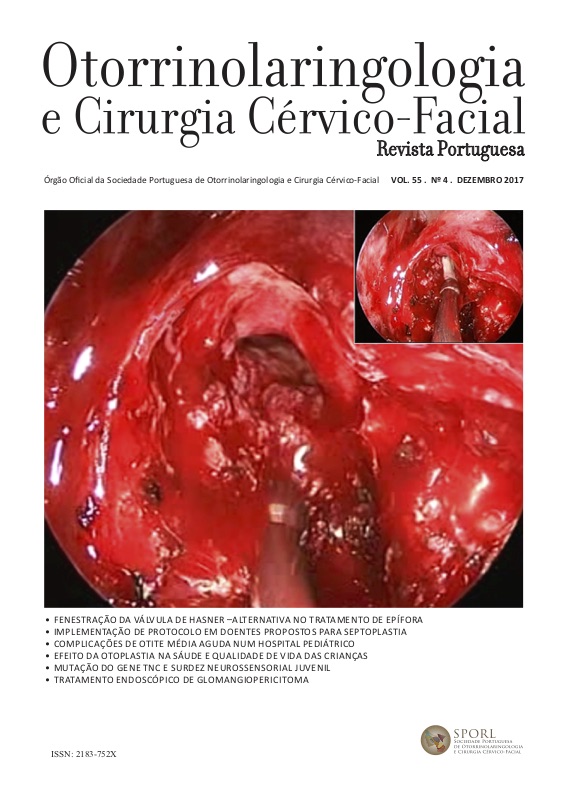
Methods: Case report: 60 years old woman with 2 years symptoms of nasal obstruction and unilateral recurrent epistaxis. Anterior rhinoscopy identified a unilateral hypervascular mass that occupied the entire left nasal cavity. Imaging studies documented the presence of extensive lesion of the left nasal cavity with complete infiltration of the anterior ethmoid, limited indentation of the medial wall of the orbit, bone demineralization of the left cribriform plate and involvement of the anterior cranial fossa. The pathological diagnosis of locally advanced GPC was done preoperatively by biopsy of the lesion resulting in a self-limited epistaxis confirming the vascular nature of the lesion. We discuss the diagnostic workup, imaging and surgical approach of this tumor and a review of the literature on endoscopic treatment of these lesions.
Results: Preoperative embolization removed 90% of the vascularization of the lesion in dependence of the infraorbital artery. We performed a complete excision of the lesion by direct endoscopic transethmoidal hemi-craniectomy. No complications associated with the technique and no postoperative locoregional recurrence was reported on follow-up.
Conclusion: Endoscopic treatment of GPC is safe and effective with results superior to those described by the external approach. Preoperative embolization of these lesions is advantageous in reducing blood feeding and blood loss intraoperatively allowing a safe and well-controlled endoscopic resection.
Downloads
References
Somu L, Kumar P, Ravikumar A, Shree R. Nasal Mass: An Enigma.
jemds. 2014 Jan 1;3(69):14250–6.
Barnes L. Pathology and Genetics of Head and Neck Tumours. World
Health Organization; 2005. 1 p.
Wang C-C. Glomangiopericytoma of Nasal Cavity: A Rare Sinonasal
Perivascular Tumor. JMS. Mathematical Association of America; 2013
Oct 1;2(33):107–11.
Stout AP, Murray MR. Hemangiopericytoma: a vascular tumor
featuring Zimmermann's pericytes. Annals of Surgery. 1942
Jul;116(1):26–33.
Thompson LDR, Miettinen M, Wenig BM. Sinonasal-type
hemangiopericytoma: a clinicopathologic and immunophenotypic
analysis of 104 cases showing perivascular myoid differentiation. Am J
Surg Pathol. ebscoatoz; 2003 May 31;27(6):737–49.
Duval M, Hwang E, Kilty SJ. Systematic review of treatment and
prognosis of sinonasal hemangiopericytoma. Eisele DW, editor. Head
Neck. 2012 Jun 25;35(8):1205–10.
Vijayasundaram S, Karthikeyan P, Coumare VN, Bakshi SS, Pulimoottil
DT. A rare case of glomangiopericytoma of the nasal cavity. Int J Cur
Res Rev. 2014 Sep 30;6(19):1–5.
Gillman G, Pavlovich JB. Sinonasal hemangiopericytoma.
Otolaryngology - Head and Neck Surgery. 2004 Dec 1;131(6):1012–3.
Tessema B, Eloy JA, Folbe AJ, Anstead AS, Mirani NM, Jourdy DN,
et al. Endoscopic management of sinonasal hemangiopericytoma.
Otolaryngology - Head and Neck Surgery. SAGE Publications; 2012
Mar;146(3):483–6.
Kamath PM, Shenoy SV, Nirupama M, Raj TV. Hemangiopericytoma:
A rare sinonasal tumor. Egyptian Journal of Ear, Nose, Throat and
Allied Sciences. Egyptian Society of Ear, Nose, Throat and Allied
Sciences; 2013 Jul 1;14(2):151–4.
Lasota J, Felisiak-Golabek A, Aly FZ, Wang Z-F, Thompson
LDR, Miettinen M. Nuclear expression and gain-of-function
beta;-catenin mutation in glomangiopericytoma (sinonasal-type
hemangiopericytoma): insight into pathogenesis and a diagnostic
marker. Nature Publishing Group; 2014 Nov 28;:1–6.
Chihani M, Aljalil A, Touati M, Zoubeir Y, Labraimi A, Ammar H,
et al. Glomangiopericytoma: An uncommon sinonasal perivascular
tumor with particular characteristics. Egyptian Journal of Ear, Nose,
Throat and Allied Sciences. Egyptian Society of Ear, Nose, Throat and
Allied Sciences; 2011 Nov 1;12(3):167–70.
Li X-Q, Hisaoka M, Morio T, Hashimoto H. Intranasal pericytic
tumors (glomus tumor and sinonasal hemangiopericytoma-like
tumor): report of two cases with review of the literature. Pathol Int.
Apr 30;53(5):303–8.
Jung ES, Yang S-W, Kim J-H, Kim SW. A case of glomangiopericytoma
involving the orbital wall. Ear Nose Throat J. 2013 Apr;92(4-5):E13–5.
Sun Q, Zhang C, Chen W, He Y. The molecular mechanisms on
glomangiopericytoma invasion. Orphanet Journal of Rare Diseases.
Orphanet Journal of Rare Diseases; 2013 Sep 29;8(1):1–1.
Angouridakis N, Zaraboukas T, Vital J, Vital V. Sinonasal
hemangiopericytoma of the middle turbinate: a case report and brief
review of the literature. B-ENT. 2007;3(3):139–43.
Verim A, Kalaycik Ertugay C, Karaca CT, Gunes P, Sheidaei S, Oysu
C. Case Report: A Rare Tumor of Nasal Cavity: Glomangiopericytoma.
Case Reports in Otolaryngology. Hindawi Publishing Corporation;
Jul 20;:1–3.
Sugimoto T, Masuda T, Uemura T, Tsuneyoshi M.
Hemangiopericytoma-like intranasal tumor: A case report with an
immunohistochemical study. Otolaryngology - Head and Neck Surgery.
;113(3):323–7.
Lin I-H, Kuo F-Y, Su C-Y, Lin H-C. Sinonasal-type hemangiopericytoma
of the sphenoid sinus. Otolaryngology - Head and Neck Surgery. 2006
Dec 1;135(6):977–9.
de Liz Medeiros AI, Selonke I, Zimmermann E. Myopericytoma in
Nasal Cavity. 2009.